Latin America, like every other region in the world, is experiencing the effects of population aging. However, aging in Latin America has unique characteristics and these characteristics point towards aspects of aging where most attention from healthcare providers and most attention from policy makers and advocates is required. In Latin American and the Caribbean, populations turning 60 years of age after the year 2000 will be particularly fragile because they survived unfavorable conditions in early childhood. Most countries in this region are developing and experienced rapid mortality decline beginning in 1930 or 1940 that was characterized by the spread of medical knowledge and technology and to a much lesser degree, by improvements in standards of living. This mortality decline, added to changes in life styles and exposure to substances, produced three outcomes: first, a decrease in the level of communicable diseases and a corresponding increase in the proportional contribution of non-communicable conditions; second, an increase in frailty of cohorts born right before, during and shortly after the implementation of medical advances; and third, a persistence of communicable diseases because root causes like limited access to clean water, poor education, and insufficient health coverage and health services that can provide preventive measures, still prevail. These outcomes put vulnerable populations, such as older adults, at higher risk of disease, disability and mortality.
These demographic characteristics of aging in Latin America place older adults in a very difficult situation. Despite the protective role of extended families in the care of older adults, specialized care is limited and policies targeted at protecting vulnerable older adults are limited and take a long time to get implemented. The number of Geriatrics programs is limited and the shortage of Geriatricians is one of the largest compared to other regions in the world. Even worst, there are many countries in Latin America that don’t have Gerontology programs. The number of healthcare providers trained in the care of older adults is therefore very limited and unlikely to improve in the near future.
In a globalized era like the one we currently live in, regional problems like the one presented above have a toll not only on the region but worldwide. The US Census projects that Hispanics will be the largest population group in the United States in the near future. This group will bring all the problems previously presented and pose an important health challenge for developed countries where migration usually occurs.
As researchers and healthcare providers we need to study these problems and conduct cross-national comparisons that may help us design policies and interventions that can help older adults have better quality of life. As a society we are not ready for the Aging Revolution that is coming upon us. Even worse we are assuming that aging follows a single pattern around the world. We must understand the unique characteristics, different countries and regions have and develop our interventions based on these unique characteristics.
This week’s Guest Blogger is Rafael Samper-Ternent M.D., Ph.D. He is currently a researcher at the aging institute at Javeriana University in Bogota, Colombia. Previously he was a fellow at the Sealy Center on Aging at UTMB.
Join us for a real-time discussion about questions raised by this essay on Tuesday from 12:00 p.m. to 12:45 p.m. See Discussion and SL tabs above for details. Link to the virtual meeting room: http://tinyurl.com/cjfx9ag.
References
- Palloni,A., & McEniry,M. (2007). Aging and health status of elderly in Latin America and the Caribbean: preliminary findings. J.Cross.Cult.Gerontol, 22(3), 263-285.
- Palloni,A., Pinto-Aguirre,G., & Pelaez,M. (2002). Demographic and health conditions of ageing in Latin America and the Caribbean. International Journal of Epidemiology, 31(4), 762-771.
- US CEnsus Bureau 2010
- Wong,R., Espinoza,M., & Palloni,A. (2007). Mexican older adults with a wide socioeconomic perspective: health and aging. Salud Publica de Mexico, 49 Suppl 4 S436-S447.



 I was thinking thankfulness yesterday. Well, first I was thinking. “Time to split logs for firewood as it’s going to be cold and rainy tomorrow.”
I was thinking thankfulness yesterday. Well, first I was thinking. “Time to split logs for firewood as it’s going to be cold and rainy tomorrow.” I was thinking about people who start to act old when they are still quite young. This phenomena was more obvious to me when I was a kid. I recall friends of my parents who really acted old when they were actually under sixty. Now, my generation has aged slower than my parents’ generation (60 is the new 40) so some of that “acting old” was probably physiological but I really think a lot of it was psychological in origin.
I was thinking about people who start to act old when they are still quite young. This phenomena was more obvious to me when I was a kid. I recall friends of my parents who really acted old when they were actually under sixty. Now, my generation has aged slower than my parents’ generation (60 is the new 40) so some of that “acting old” was probably physiological but I really think a lot of it was psychological in origin. The magic of creating of intelligent machines that could interact with humans has long fascinated us (1). Early attempts were based on clockwork mechanisms and called Automatons. Fritz Lang, in his 1927 film Metropolis, created the ultimate mechanical woman who looked quite natural and fooled others that it was human (2). As a child, I first saw a robot in the film Forbidden Planet back in the middle 1950’s (3) provided we discount the Tin Man from the Wizard of Oz whom I did see earlier. I even developed a screenplay for a film about a woman with an artificial, sentient hand but that’s another story.
The magic of creating of intelligent machines that could interact with humans has long fascinated us (1). Early attempts were based on clockwork mechanisms and called Automatons. Fritz Lang, in his 1927 film Metropolis, created the ultimate mechanical woman who looked quite natural and fooled others that it was human (2). As a child, I first saw a robot in the film Forbidden Planet back in the middle 1950’s (3) provided we discount the Tin Man from the Wizard of Oz whom I did see earlier. I even developed a screenplay for a film about a woman with an artificial, sentient hand but that’s another story. What I found interesting about Robot & Frank was how naturally Frank, after some initial rejection, began to treat the robot as a person. I know I talk back to the navigation computer in my car, so I see how easily we anthropomorphize things.
What I found interesting about Robot & Frank was how naturally Frank, after some initial rejection, began to treat the robot as a person. I know I talk back to the navigation computer in my car, so I see how easily we anthropomorphize things.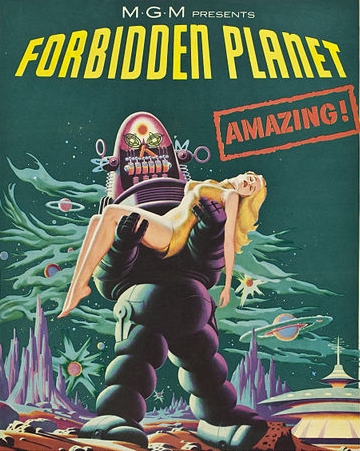
 I had breakfast this morning with some friends at the Wimberley Café. It’s one of those local hangouts where you are sure to see someone you know. On this occasion, my neighbor, who lives about a quarter mile up the hill from me, was at the next table.
I had breakfast this morning with some friends at the Wimberley Café. It’s one of those local hangouts where you are sure to see someone you know. On this occasion, my neighbor, who lives about a quarter mile up the hill from me, was at the next table. The East Texas Geriatric Education Center-Consortium (ETGEC-C) hosts a monthly video series focusing on a wide range of aging topics. Some videos are light and fun, such as Quartet, Young at Heart and Age of Champions. Others are educational, like Exploring the Myths of Dementia. And then there are those that tear at the heart and make you wonder what it will be like when you are old, fragile and need help. Today we had one of those videos. Living Old is a PBS Frontline film from 2006 that looks at the challenges facing America’s growing elderly population. The film’s synopsis states “those over the age of 85 now comprise the fastest growing segment of the U.S. population, creating a much higher need for medical care and straining America’s health care system.”
The East Texas Geriatric Education Center-Consortium (ETGEC-C) hosts a monthly video series focusing on a wide range of aging topics. Some videos are light and fun, such as Quartet, Young at Heart and Age of Champions. Others are educational, like Exploring the Myths of Dementia. And then there are those that tear at the heart and make you wonder what it will be like when you are old, fragile and need help. Today we had one of those videos. Living Old is a PBS Frontline film from 2006 that looks at the challenges facing America’s growing elderly population. The film’s synopsis states “those over the age of 85 now comprise the fastest growing segment of the U.S. population, creating a much higher need for medical care and straining America’s health care system.” I couldn’t get pregnant because I was missing some critical organs. It was a very dark period in my life – being faced with a health situation that was out of my control. My doctor, let’s call her Dr. Nassairia, was very tough and serious. She didn’t have many warm words of comfort, but at the end of countless appointments, she always patted my knee and smiled into my eyes. I called it the Nassairia knee pat. It wasn’t much, but her demonstration of empathy was just enough to keep me going.
I couldn’t get pregnant because I was missing some critical organs. It was a very dark period in my life – being faced with a health situation that was out of my control. My doctor, let’s call her Dr. Nassairia, was very tough and serious. She didn’t have many warm words of comfort, but at the end of countless appointments, she always patted my knee and smiled into my eyes. I called it the Nassairia knee pat. It wasn’t much, but her demonstration of empathy was just enough to keep me going. Living in the rural Texas Hill Country I get my electricity from the Pedernales Electric Cooperative. This is a private electric utility owned by the members it serves. It was established in 1938 as part of the Rural Electrification Administration.
Living in the rural Texas Hill Country I get my electricity from the Pedernales Electric Cooperative. This is a private electric utility owned by the members it serves. It was established in 1938 as part of the Rural Electrification Administration. As the Social Worker in the Out-patient clinics at UTMB I both look forward to and dread this time of the year. Medicare Open Enrollment is a confusing and overwhelming time for seniors and their families. Last year I assisted more than 120 patients review their Medicare enrollments. I look forward to this time because our patients are able to get out of plans that do not work for them anymore. I dread it because there are many uninformed people giving seniors advice that is not correct and sometimes the senior is stuck with the wrong plan until next year.
As the Social Worker in the Out-patient clinics at UTMB I both look forward to and dread this time of the year. Medicare Open Enrollment is a confusing and overwhelming time for seniors and their families. Last year I assisted more than 120 patients review their Medicare enrollments. I look forward to this time because our patients are able to get out of plans that do not work for them anymore. I dread it because there are many uninformed people giving seniors advice that is not correct and sometimes the senior is stuck with the wrong plan until next year.
 Spending a week at the lake house in East Texas this summer, I ran into some older gentlemen whose lives revolve around bass fishing and boating on the lake. Everyone who spends a lot of time on the water shares a concern about exposure to the sun. When I enquired about application of sunscreen, none of them admitted to using sunscreen as a protection. They did not think that sunscreen is very effective with the amount of time they spend outside, sweating and in and out of the water. They all had stories of friends and family members with a history of skin cancers.
Spending a week at the lake house in East Texas this summer, I ran into some older gentlemen whose lives revolve around bass fishing and boating on the lake. Everyone who spends a lot of time on the water shares a concern about exposure to the sun. When I enquired about application of sunscreen, none of them admitted to using sunscreen as a protection. They did not think that sunscreen is very effective with the amount of time they spend outside, sweating and in and out of the water. They all had stories of friends and family members with a history of skin cancers. Ronald Crossno recently published an opinion piece in the Austin American Statesman (8-28-13) about several bills in Congress aimed at increasing the number of healthcare professionals trained to provide hospice services. The bills are: Palliative Care and Hospice Education and Training Act (H.R. 1339 and S. 641) and Patient Centered Quality Care for Life Act (H.R. 1666). These bills, if passed, would provide Federal support for training and various other activities aimed at increasing the availability of palliative care.
Ronald Crossno recently published an opinion piece in the Austin American Statesman (8-28-13) about several bills in Congress aimed at increasing the number of healthcare professionals trained to provide hospice services. The bills are: Palliative Care and Hospice Education and Training Act (H.R. 1339 and S. 641) and Patient Centered Quality Care for Life Act (H.R. 1666). These bills, if passed, would provide Federal support for training and various other activities aimed at increasing the availability of palliative care. Mary was a great patient. She came in regularly, every six months. Nothing wrong, just wanted to make sure everything was working fine. It always was. On this Monday though, something was ever so slightly off. Mary’s gait was wobbly. She was talking just a little too slowly. “What’s wrong?” I asked. She tried to smile. “Nothing, only…” The pause told me what I wanted to know, but I waited for her to finish. “Only the last few days…” Eventually it came out. Her new regimen of morning grapefruit juice was amplifying the effects of her blood pressure medications.
Mary was a great patient. She came in regularly, every six months. Nothing wrong, just wanted to make sure everything was working fine. It always was. On this Monday though, something was ever so slightly off. Mary’s gait was wobbly. She was talking just a little too slowly. “What’s wrong?” I asked. She tried to smile. “Nothing, only…” The pause told me what I wanted to know, but I waited for her to finish. “Only the last few days…” Eventually it came out. Her new regimen of morning grapefruit juice was amplifying the effects of her blood pressure medications. Our Guest Blogger this week is Mukaila Raji, M.D., M.S., F.A.C.P. Professor & Director, Division of Geriatric Medicine, Edgar Gnitzinger Distinguished Professorship in Aging, and Program Director, Geriatric Medicine Fellowship
Our Guest Blogger this week is Mukaila Raji, M.D., M.S., F.A.C.P. Professor & Director, Division of Geriatric Medicine, Edgar Gnitzinger Distinguished Professorship in Aging, and Program Director, Geriatric Medicine Fellowship “Driving by men has declined in every age group except those 65 or older, where it increased slightly. Among women, driving declined only among young adults and teenagers.”
“Driving by men has declined in every age group except those 65 or older, where it increased slightly. Among women, driving declined only among young adults and teenagers.”
 We are accustomed to the routine measurement of blood pressure, heart rate, respiratory rate, and temperature at every visit to the doctor’s office. We are not surprised by 4:00 am awakenings for obligatory vital sign monitoring in a hospital. Since 2001, the Joint Commission on Accreditation of Healthcare Organizations has required pain assessment in healthcare settings (1). Thus, pain is commonly referred to as a 5th vital sign. What will be the 6th vital sign? Some suggestions include: health-related quality of life (2), distress (3), health literacy (4), urinary incontinence (5), mental status (6), fall risk (7), and gait speed (8). All of these factors are particularly relevant to aging adults. I will elaborate on gait speed, and perhaps future bloggers will be inspired to explore other potential 6th vital signs.
We are accustomed to the routine measurement of blood pressure, heart rate, respiratory rate, and temperature at every visit to the doctor’s office. We are not surprised by 4:00 am awakenings for obligatory vital sign monitoring in a hospital. Since 2001, the Joint Commission on Accreditation of Healthcare Organizations has required pain assessment in healthcare settings (1). Thus, pain is commonly referred to as a 5th vital sign. What will be the 6th vital sign? Some suggestions include: health-related quality of life (2), distress (3), health literacy (4), urinary incontinence (5), mental status (6), fall risk (7), and gait speed (8). All of these factors are particularly relevant to aging adults. I will elaborate on gait speed, and perhaps future bloggers will be inspired to explore other potential 6th vital signs. 2013;66:706-709.
2013;66:706-709. The United States is one of the few countries in the world that considers health care as a commodity and pays for it through the mechanism of insurance provided by private corporations. The rest of the world considers health care to be a public service. Why don’t we change?
The United States is one of the few countries in the world that considers health care as a commodity and pays for it through the mechanism of insurance provided by private corporations. The rest of the world considers health care to be a public service. Why don’t we change? “Avoidance is the most straightforward way of dealing with conflicts of interest.”
“Avoidance is the most straightforward way of dealing with conflicts of interest.”